Patients with spots of diminished or no vision (scotomas) often do not realize the nature of their deficit. This technique can help patients to heighten their awareness of scotomas.
In the process of learning eccentric viewing, several stages have to be passed:
1. Patients use their own hand movements to find the location of best vision in the visual field of one eye, while the other eye is closed and gaze is fixed.
2. Patients use eye movements to adjust gaze so that a target in a stable location looks best.
3. Coordinate eye and hand movements, so that a magnifier can be moved where it is needed, namely at the location in the visual world that correspond to a Preferred Retinal Locus (PRL).
The techniques described here serves the purpose of stage 1 (above). We have developed two techniques to solve this problem. In both cases, the examiner has to guess in which quadrant of the visual field the spot of best vision can be expected. This is possible by two simple techniques:
A. While examiner and patient confront each other, the patient is asked to look at the examiner’s nose. This allows the examiner to see the deviation of the patient’s gaze. Example: If the patient looks slightly up and right, the examiner can conclude that the patient is using a spot in the lower left of the visual field.
B. Conduct a simple topographic test of the patient’s visual field like the Macular Mapping Test (see "Macular Mapping Test", this website) or a tangent screen test. The results will indicate where relatively intact vision is available.
After these preliminary tests, the screen or card (see below) should show free space in the quadrant indicated by the visual field test.
Visual Field Self-Exploration
A. The scientific (“high-tech”) way: This technique uses a computer, a monitor and a light pen. The patient looks at the right angle between two straight high contrast edges using the center of the retina. This is done even if the angle itself is seen blurred or disappears altogether due to a scotoma. Gaze should be held as stable as possible.
Simultaneously, the patient moves their preferred hand holding a small light pen over the monitor screen. The light pen automatically moves a letter where ever the hand moves. The patient explores the visual field to examine changes in how the letter is seen: Sometimes clear, sometimes blurred, or sometimes not at all. When the patient reports the location of best vision, the examiner takes a note of it. (see part A in Figure below)
B. The practical (“low tech”) way: This is done with the help of a cardboard sheet that again shows a right angle between two straight high contrast edges. The preferred hand is used to move a small piece of cardboard with a letter printed on it through the visual field. Thus, the field can be explored in the same way described above for the “high tech” method.
Normal.dotm 0 0 1 470 2680 SKERI 22 5 3291 12.0 0 false 18 pt 18 pt 0 0 false false false /* Style Definitions */ table.MsoNormalTable {mso-style-name:"Table Normal"; mso-tstyle-rowband-size:0; mso-tstyle-colband-size:0; mso-style-noshow:yes; mso-style-parent:""; mso-padding-alt:0in 5.4pt 0in 5.4pt; mso-para-margin:0in; mso-para-margin-bottom:.0001pt; mso-pagination:widow-orphan; font-size:12.0pt; font-family:"Times New Roman"; mso-ascii-font-family:Cambria; mso-ascii-theme-font:minor-latin; mso-fareast-font-family:"Times New Roman"; mso-fareast-theme-font:minor-fareast; mso-hansi-font-family:Cambria; mso-hansi-theme-font:minor-latin;}
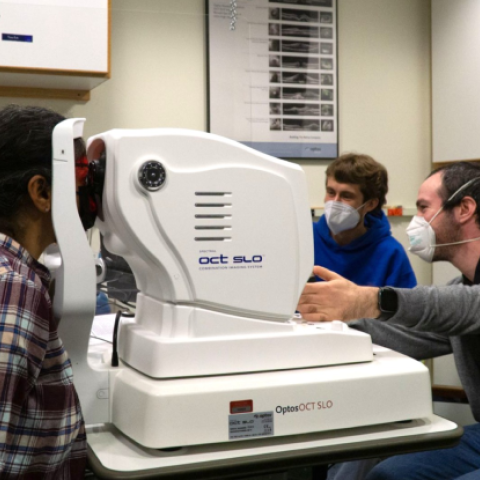
Our experience with patients shows that they take to this procedure with interest and often with enthusiasm. We have also tested these methods against results of an examination by Scanning Laser Ophthalmoscope (SLO), which shows the location of a PRL with great precision. (see part B in Figure below)